Dementia Care: Caregiving Tips to Help a Parent Living with Dementia
How to navigate dementia diagnosis, finances, safety, and care planning for a loved one
Studies have consistently shown that proactive management of Alzheimer’s and other dementias can improve the quality of life for individuals and their caregivers. Data published in the 2022 Alzheimer’s Disease Facts and Figures report that 83 percent of the help provided to older adults in the United States comes from family members, friends, or other unpaid caregivers, with more than 11 million Americans providing unpaid care for people with Alzheimer's or dementia.
This number represents an average of 27.1 hours of care per caregiver per week or 1,413 hours per caregiver per year. This forms an estimated 16 billion hours of informal assistance, a contribution to the nation valued at $271.6 billion.
From helping with a diagnosis to managing finances and looking after their mental health, there is a lot for a caregiver to consider. The impact of the disease can be minor in the early stages, but as it advances, your loved one will need more help with daily tasks. Making a dementia care plan can ensure your loved one lives a fulfilling life while protecting your mental health from potential caregiver burnout.
How to Manage a Diagnosis for a Loved one with Dementia
When there are common signs of dementia, such as memory loss, forgetfulness, confusion, peculiar financial decisions, and unusual expenditure, you should ask your loved one to speak with a medical professional. Doctors can perform tests to rule out other potential causes and if necessary, confirm a dementia diagnosis.
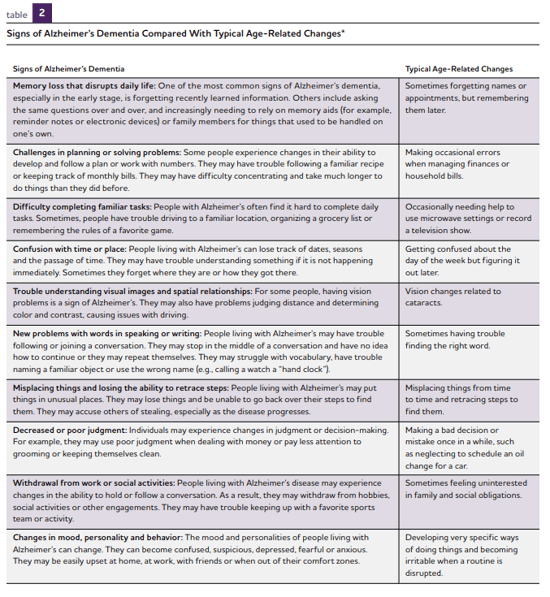
The table below from alz.org provides an overview of 10 common early signs of Alzheimer’s and the difference from typical age-related changes in behavior.
Dealing with the emotional impact of dementia or Alzheimer’s diagnosis can be challenging for your loved one and their family members. It’s important at this time to remain positive - there are no cures for dementia, but medications can help manage the symptoms. With care planning in place, a dementia patient can still enjoy an active and social life for years after a diagnosis.
It’s also important to realize that you will not be alone as a caregiver. Caregiving can seem overwhelming after the diagnosis, as the impact on your personal life, career, finances, and social life comes into question. Most Alzheimer’s and dementia patients receive help from multiple family members, doctors, and community support organizations.
After a diagnosis, it can be beneficial to provide as much routine as possible for the dementia patient, who may be struggling with varying degrees of forgetfulness and challenges with thinking and reasoning.
Consider implementing some of the tips below, as suggested by Alzheimer.gov:
- Set bathing, dressing, and eating at the same time each day.
- Write down the schedule and events in a calendar.
- Plan enjoyable activities to repeat on the same day and time.
- Implement a reminder system for taking regular medications.
Dementia Care Finances: Looking after the Financial Well-being of Alzheimer's Patients
Those with dementia or Alzheimer's are more vulnerable than others on legal and financial issues. They may cause unintentional harm to their own financial or legal plans due to the effects of dementia, or be vulnerable to others acting in bad faith who may try to take advantage of them for financial gain.
According to the Alzheimer’s Association, caregivers can help to protect their loved ones by putting plans in place soon after a diagnosis, with the input of the dementia patient. They say:
“Putting financial and legal plans in place now allows the person with dementia to express wishes for future care and decisions. It also allows time to work through the complex issues involved in long-term care.”
Aside from protecting the finances of the care recipient, the caregiver needs to consider the financial impact of providing support for someone with dementia and if the resources are in place to pay for doctors, medications, home care, safety modifications, or general household living expenses for their loved one. It may be a difficult discussion, but the caregiver should ask their loved one for access to financial and insurance policy details so they can understand what is already in place.
Here are a few practical tips on managing the finances of a loved one with dementia:
- Ask for permission. As a caregiver, you will contact insurance companies, doctors, and hospitals on behalf of your loved one. Ask for permission to share information between yourself and the other parties.
- Ask for access. Ask your loved one for access to finances, bank accounts, and for details on bills. Monitor financial accounts for unusual transactions and signs of financial abuse to help protect your loved one.
- Take care of legal issues. Your loved one should designate a power of attorney after a diagnosis of dementia. Should they not do this and later become incapable of making a decision, the matter will need intervention from the courts.
How to Create a Dementia Caregiving Plan for Your Loved One
Creating a proactive caregiving plan to manage the dementia of a parent or loved one can help improve the lives of everyone involved.
An effective caregiving plan involves gaining a more comprehensive understanding of the condition, managing the available treatment options, coordinating a caregiving team effort, and planning activities that create a meaningful life for your loved one.
Educating yourself on Alzheimer’s and dementia is an important first step. While you can’t anticipate everything that will happen you can understand the different stages, progression, and best treatment and lifestyle options, so you and your fellow caregivers can prepare as best as possible.
Part of your caregiving plan will be collaborating with your loved one and medical professionals to discuss appropriate treatment options. This is something you will review periodically as the condition changes over time. Caregivers should consider the effective management of coexisting conditions and medications alongside Alzheimer’s treatment.
If your caregiving team consists of multiple members, organizing a schedule and training others on medication or other daily caregiving tasks may be required. Managing medical appointments, preparing meals, grocery shopping, collecting prescriptions, and paying bills are some of the tasks that need to be assigned across the caregiving team.
An important part of a dementia caregiving plan is providing participation in activities that are meaningful to the individual with dementia. Listen to your loved one and allow them to participate in discussions about their needs, plans, and enjoyable activities. This could include helping them to maintain a sense of self-identity and relationships with others, such as connecting with others living with dementia via support groups. You can also encourage other relatives to stay connected to your loved one to help alleviate isolation and loneliness.
Caregivers should also plan for the future. Alzheimer's and dementia may change or worsen, an emergency might occur after an accident, and future planning can help caregivers react quickly.
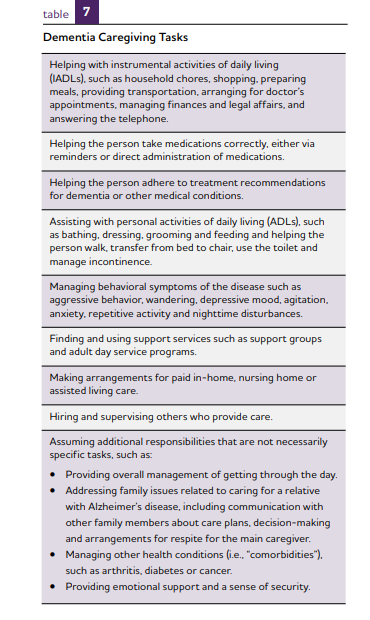
The table below from alz.org provides an overview of the dementia caregiving tasks you may need to provide.
How to Manage Dementia Health and Safety Risks at Home
According to DementiaUK, making changes to the home of a person with dementia can make it safer and more comfortable for them to remain at home.
“To help a person with dementia maintain their independence and quality of life, it’s important to make their home as safe and comfortable as possible. This needn’t be expensive or disruptive – small changes often make a big difference.”
After a dementia or Alzheimer’s diagnosis, you will need to consider safety hazards in the home and how to prevent harm to the care recipient. To help make sure your loved one does not injure themselves, you might need to make modifications that reduce their risk of falling or wandering. Installing a hospital bed, stair lifts, or exit alarms are steps that can help manage these safety concerns.
There are other potential risks related to memory loss and confusion: taking too much medication and turning on ovens, fires, heaters, or other electrical equipment. Adding safety measures to control access to medicine and disabling the oven or fire when not needed can help provide peace of mind.
The confusion that can occur during dementia means that driving or operating machinery provides danger to the care recipient and others. Ask for help discussing this with your loved one from medical professionals if required. Fear of losing freedom can make patients want to continue driving even when it is no longer safe.
How to Care for Yourself as a Caregiver
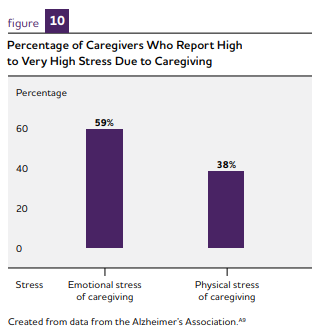
Caregiving is known to have both a physical and mental health impact on many caregivers, leading to stress, anxiety, isolation, and depression. Dementia can be emotionally difficult as it involves caregiving for a loved one whose personality and capabilities may have changed significantly.
Many caregivers face multiple pressures, including balancing work, family life, and caregiving with added financial demands. According to a study by the National Alliance for Caregiving in Partnership with the Alzheimer’s Association, titled Dementia Caregiving in the U.S., six in 10 caregivers of people with Alzheimer’s or another dementia were employed or had been employed in the prior year while providing care. These individuals worked an average of 35 hours per week while caregiving.
Among people who were employed in the past year while providing care to someone with Alzheimer’s or another dementia, 57 percent reported arriving at work late or leaving early compared with 47 percent of non-dementia caregivers. 18 percent of dementia caregivers reduced work hours to manage caregiving responsibilities, compared with 13 percent of non-dementia caregivers.
A research paper titled Caregiving as a risk factor for mortality: the Caregiver Health Effects Study shows that as the person with dementia symptoms worsens, caregivers can experience increased emotional stress and depression.. New health problems, depleted income and finances due in part to disruptions in employment and paying for health care are also common.
Caregivers for relatives with dementia must take time out to care for themselves, share the burden with others, and communicate with their employers about the pressures they are facing. Consider joining a support group, seeing a therapist, or taking time to do an activity that you enjoy.
Support networks are vital for dementia caregivers. Creating a network of friends, family, and neighbors provides emotional support and respite from caregiving duties. A break from caregiving can make you a stronger caregiver in the long term.
Talking therapy with a counselor can help carers suffering from anxiety or depression. Respite care is another practical solution that offers a much-needed rest from caregiving so you can take time to care for yourself, meet with other friends and family, or run errands.
At the same time, the person living with Alzheimer's continues to receive care in a safe environment and can participate in activities designed to match their personal abilities and needs.
Employers that provide a caregiving support package can point employees to expert caregiving advice to help them navigate the challenges ahead. With a mortality rate increasing almost 150 percent in the past 20 years, 1 in 3 adults die from Alzheimer’s or another dementia (Alzheimer’s Association, 2022) which means many of us will increasingly be affected by Alzheimer's disease and dementia.
